Patients of all ages experience loss and grief. For older adults, that can be the loss of a loved one, a career, independence, or a decline in health. In a Q&A with Vytalize’s Behavioral Health Registered Nurse (RN) Case Managers, Richie S., BSN, RN-BC and Sharon Dougherty, RN, LCSW-R, we explore grief’s impact on older adults, coping techniques and ways value-based care can provide a way forward.
 How does grief impact a patient’s day to day, and do you find that it impacts a patient’s desire or willingness to seek care?
How does grief impact a patient’s day to day, and do you find that it impacts a patient’s desire or willingness to seek care?
Richie: Grief can significantly affect how patients go about their daily lives, causing emotions like sadness and anger that can disrupt their routines and decision-making. In my nine years as a board-certified mental health nurse, I’ve noticed that grief can make patients hesitant to seek help. Some may view their grief as a natural reaction to loss, while others fear that discussing it might intensify their pain. The energy drain and isolation tied to grief can further discourage them from seeking assistance.
As a Behavioral Health RN Care Manager, I create a supportive space where patients understand that seeking care is a brave step toward healing, adapting interventions to their pace and needs. It’s important to respect individual journeys through grief and guide patients toward the care and support they need.
Sharon: Grief influences every aspect of a person’s life. Depending on the role the loved one plays in the patient’s lifetime, it can be a major impact. In the case of a lost spouse, or another significant family member, the loss may be much stronger than in the case of a distant relative or acquaintance. Even the loss of a pet can be very significant, more so than some relatives. We not only grieve the loss of the person or, but all the roles they played in our life – best friend, lover, confidant, housekeeper, family bookkeeper, baby, etc. The more significant the lost one was to your life, the greater the impact.
As my colleague pointed out, people are often afraid to discuss the deceased to avoid upsetting them. It has been my experience that the person wants to talk about their loss – to know that their loved one did not die in vain and that they touched others as well. This is very important for grieving.
As an RN and Clinical Social worker, I have had the opportunity to help many adjust to their loss. One never “gets over it;” rather, they just learn to manage the grief. I have watched many patients leave this earth, and then the subsequent impact on the family and each person’s response to the loss. Some feel they need to protect other family members and try to be stoic, while others may not understand that we all have our own timelines for grief. Even if we are feeling better, a silly song, special date, or brand of coffee can put us into hysteria.
Being a young widow myself, I understand how one’s life can be turned upside down in an instant, and how unimaginable it is that life just goes on for everyone else. In my 30+ years of practice, I have found that patients are most comfortable when you validate their loss, as well as their pain. This helps people feel more comfortable sharing. I allow them to control how much is shared and go at their pace. No two situations are identical, but if the pain is understood and acknowledged, people are more apt to open up.
As we age, the loss of loved ones becomes more common. What is that experience like for patients and are there other contributing factors to their grief?
Richie: Subsequent losses can be a complex and challenging experience for patients, which can factor into their grief response. Beyond the emotional impact of grief, there are other factors that contribute to their feelings. These include changes in physical health, social connections, and life roles. Coping with these losses can vary based on an individual’s support network, personal resilience, and cultural background. As a result, the aging process involves navigating a web of emotions and adjustments, which requires a sensitive and individualized approach from caregivers and healthcare professionals.
Sharon: As time goes on, we soon learn that many people who we once were close to are no longer there. With the simple aging process and medical conditions that often accompany it, older people tend to isolate people more and more. We begin to realize that our time here is limited, and sometimes people feel guilty about wanting the suffering to end for a loved one but think badly of themselves for “wishing their loved one dead.” Being supportive and understanding is crucial to assist with grieving. I often recommend community or parochial support groups (as appropriate) to parents and widows, where there is comfort in sharing a similar experience. This also offers opportunities for socializing and developing a new bond with understanding or single friends.
What are some maladaptive behaviors that may come with grief, and what are other signs providers and caregivers should look out for?
Richie: Providers and caregivers should be vigilant for certain signs when assessing patients who are grieving. These signs might include persistent feelings of hopelessness, prolonged social withdrawal, significant changes in appetite or sleep patterns, and a loss of interest in activities that were once enjoyable. Additionally, expressions of intense guilt, difficulty in focusing, or a lack of motivation might indicate a more challenging grief process.
Maladaptive behaviors can also emerge in response to grief. These behaviors might involve excessive substance use, prolonged isolation, and a refusal to engage with support systems. Some individuals may become overly preoccupied with thoughts of the deceased, avoiding situations that remind them of the loss. It’s important to note that these reactions can vary widely from person to person, and not everyone will exhibit the same signs or behaviors. Understanding these potential signs and behaviors allows providers and caregivers to intervene appropriately and provide the necessary support to individuals navigating their grief journey.
What’s the difference between grief and clinical depression?
Richie: Grief and clinical depression share some common emotional features, yet they diverge significantly in their origins and clinical presentation. Grief arises as a natural reaction to a significant loss, encompassing emotions like sadness, anger, and yearning. These emotions can impede cognitive processes and disrupt daily functioning.
In contrast, clinical depression is a distinct psychiatric disorder that may manifest independently of any identifiable loss. Characterized by persistent low mood, anhedonia, sleep and appetite disturbances, and pervasive feelings of worthlessness or guilt, clinical depression transcends situational triggers and profoundly affects an individual’s psychosocial and functional well-being. Discerning grief from clinical depression is pivotal in ensuring appropriate interventions tailored to the underlying condition.
To oversimplify it, grief and clinical depression have similarities, but they’re different. Grief comes from losing something important and brings sadness and anger. Clinical depression is a medical disorder with ongoing sadness, loss of interest, and problems with sleep, eating, and self-worth.
What are some coping tips that you can share with patients and their caregivers?

Richie: Some coping tips for both patients and their caregivers that make a positive impact are:
- Communication: Open and honest conversations among family members and caregivers can foster understanding and support. Sharing thoughts and feelings helps everyone feel heard and reduces isolation.
- Self-Care: Encourage patients and caregivers to prioritize self-care. Engaging in activities they enjoy, maintaining routines, and focusing on physical health through proper sleep, nutrition, and exercise can contribute to emotional well-being.
- Support Groups: Connecting with others who have experienced similar situations can provide a sense of belonging and validation. Support groups offer a safe space to share emotions and coping strategies.
- Mindfulness and Relaxation: Practices like deep breathing, meditation, and mindfulness exercises can help manage stress and anxiety. These techniques promote a sense of calm and improve emotional resilience.
- Seeking Professional Help: For patients, working with mental health professionals can provide tailored strategies and tools to navigate their emotions. Caregivers should also consider seeking their own support, as caregiving can be emotionally taxing.
- Journaling: Encouraging patients and caregivers to write down their thoughts and emotions can be therapeutic. It allows for introspection, self-expression, and tracking progress over time.
- Balancing Responsibilities: Caregivers should find a balance between providing care and taking care of themselves. Setting boundaries, delegating tasks, and asking for help when needed are essential.
- Focus on Positives: Identifying even small positive aspects of the situation can promote a sense of hope. Celebrating achievements, maintaining gratitude, and finding joy in everyday moments can improve mood.
- Professional Guidance: Patients and caregivers can both benefit from speaking to mental health professionals who specialize in grief and coping with loss, and provide personalized guidance and strategies.
- Time and Patience: Grief doesn’t follow a set timeline, so being patient with oneself and allowing emotions to unfold naturally is crucial. Encouraging patients and caregivers to give themselves permission to heal at their own pace can be comforting.
As a Behavioral Health RN Care Manager, I’ve found that tailoring these coping tips to the unique needs and preferences of each patient can make a significant difference in their journey toward healing and adaptation.
Sharon: As mentioned earlier, people grieve at their own rate. Some appear to move on quickly but suffer in silence, while others become isolated and show signs of depression or sadness. A psychiatrist friend of mine once said, “you can’t medicate out grief.” However, when grief becomes too overwhelming, this may be one avenue to explore. If the person is demonstrating unhealthy or risky behavior in response to their loss, it is most appropriate to refer that person for a group or professional assistance.
How does your team work with providers to address behavioral health issues?
Richie: I work closely with providers to address behavioral health concerns, which ensures that patients receive comprehensive care. I share mental health insights, help create unified care plans, and update medical providers about changes in a patient’s mental health. I also coordinate appointments, provide educational resources, and maintain a feedback loop. This collaborative approach ensures that both mental and physical health aspects are considered, leading to improved patient outcomes.
Sharon: Many of my patients were referred to me by their primary care provider. I often share my own personal loss story as appropriate, which I have found helps patients realize that someone else profoundly relates to their grief experience and the feelings that come with it. “Surreal” is the most common description I hear about what they feel. I often say that being a widow grants you entrance to a very exclusive club, but the dues we pay to join are far too costly.
How does the value-based care model allow providers to address grief and other behavioral health issues adequately?
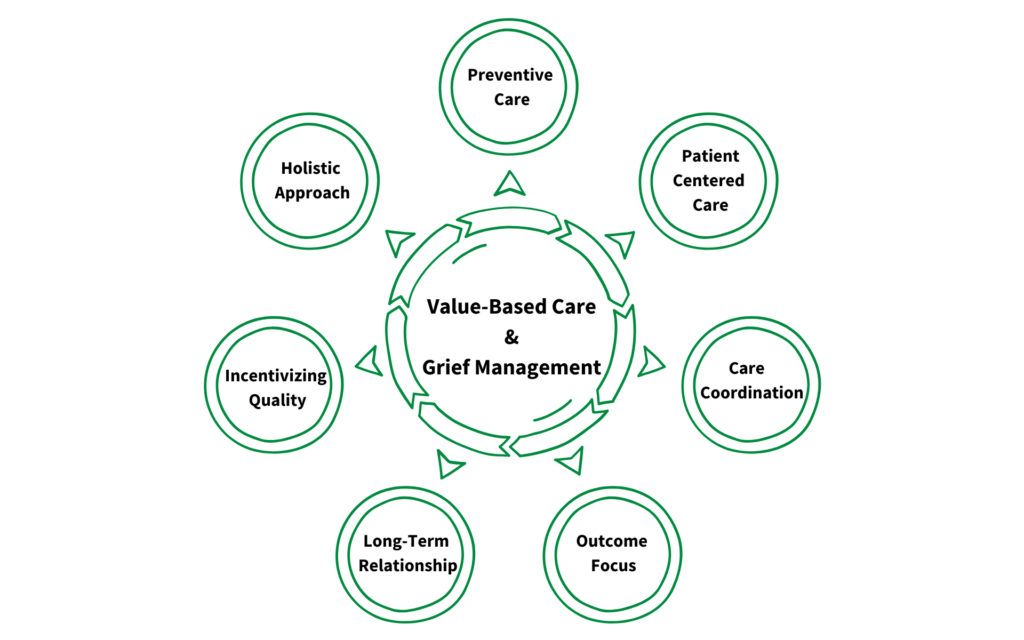
Richie: The value-based care model offers a framework that aligns well with addressing grief and other behavioral health issues effectively. Here’s why:
- Holistic Approach: The value-based care model emphasizes treating the whole person rather than focusing solely on specific conditions. Grief and behavioral health issues are interconnected with physical health. By addressing these concerns in a comprehensive manner, providers can offer more effective care that considers the patient’s emotional, mental, and physical well-being.
- Preventive Care: Value-based care encourages preventive measures and early interventions. In the context of grief, addressing emotional distress and providing coping strategies early on can prevent the development of more severe mental health issues, such as depression or anxiety, that may require hospitalization or other costly and invasive treatments. This proactive approach helps reduce the long-term burden on both patients and the healthcare system.
- Patient-Centered Care: The value-based care model places patients at the center of decision-making. By actively involving patients in their care plans and considering their preferences, providers can tailor interventions to their unique needs and cultural backgrounds. This enhances engagement and adherence to treatment, which is particularly important because individual experiences vary widely when it comes to grief.
- Care Coordination: Value-based care promotes care coordination among different healthcare providers. Behavioral health issues often coexist with a variety of medical conditions. Providers should collaborate to ensure that their shared patients receive integrated care, addressing both the physical and emotional aspects of their health.
- Outcome Focus: Value-based care places a strong emphasis on achieving positive health outcomes. In the context of grief, this means not only reducing symptoms but also improving the patient’s overall quality of life. By monitoring and measuring outcomes, providers can track the effectiveness of interventions and make necessary adjustments to optimize care.
- Long-Term Relationship: The value-based care model encourages building long-term relationships between providers and patients. This continuity of care is crucial in addressing grief, as the journey towards healing is not time-limited. Establishing a strong therapeutic alliance allows providers to support patients through the ups and downs of their grief process.
- Incentivizing Quality: Value-based care models often reward quality and patient satisfaction rather than just the quantity of services provided. This incentivizes providers to invest time in understanding the unique needs of patients dealing with grief and other behavioral health issues, leading to more personalized and effective care.
Incorporating the principles of the value-based care model into the treatment of grief and behavioral health issues allows for a more holistic, patient-centered, and outcomes-driven approach that benefits patients and the healthcare system.
Sharon: Value-based care offers us the ability to be there with and for our patients. Early support and intervention can make a difference in how well someone goes on in their “new” life without someone. A bereavement counselor once told me that it’s kind of like having a major surgery or amputation. If the wound is cared for and the dressings are cleaned and changed regularly, a scar is still there. But the wound is much cleaner, more manageable and on its way to healing.
Providers, contact us today to learn how a partnership with Vytalize Health can enable you to better manage your patients’ grief.