Every year one in five Medicare beneficiaries experience a readmission to the hospital within 30 days, costing more than $26 billion each year. More than 50% of those individuals did not have any contact with their primary care provider (PCP) after discharge, which may make it more difficult for patients to understand their instructions, follow new care plans, and avoid an exacerbation of their condition.
Every year one in five Medicare beneficiaries experience a readmission to the hospital within 30 days, costing more than $26 billion each year. More than 50% of those individuals did not have any contact with their primary care provider (PCP) after discharge, which may make it more difficult for patients to understand their instructions, follow new care plans, and avoid an exacerbation of their condition.
Primary care plays a central role in improving transitions of care (ToC). The phrase “transitions of care” is exactly as it sounds. It is a process of transferring a patient’s care from one setting or level of care to another; for example, from a hospital visit to their home.
Patients are extremely vulnerable when they move between different parts of the healthcare system. During transitions of care, PCPs often encounter care gaps that are beyond their control due to factors such as inaccessible patient records, unclear discharge care plans, or limited effort by others to engage the primary care team or the patient and his or her caregivers.
How can providers successfully handle transitions of care for their patients and help avoid readmissions?
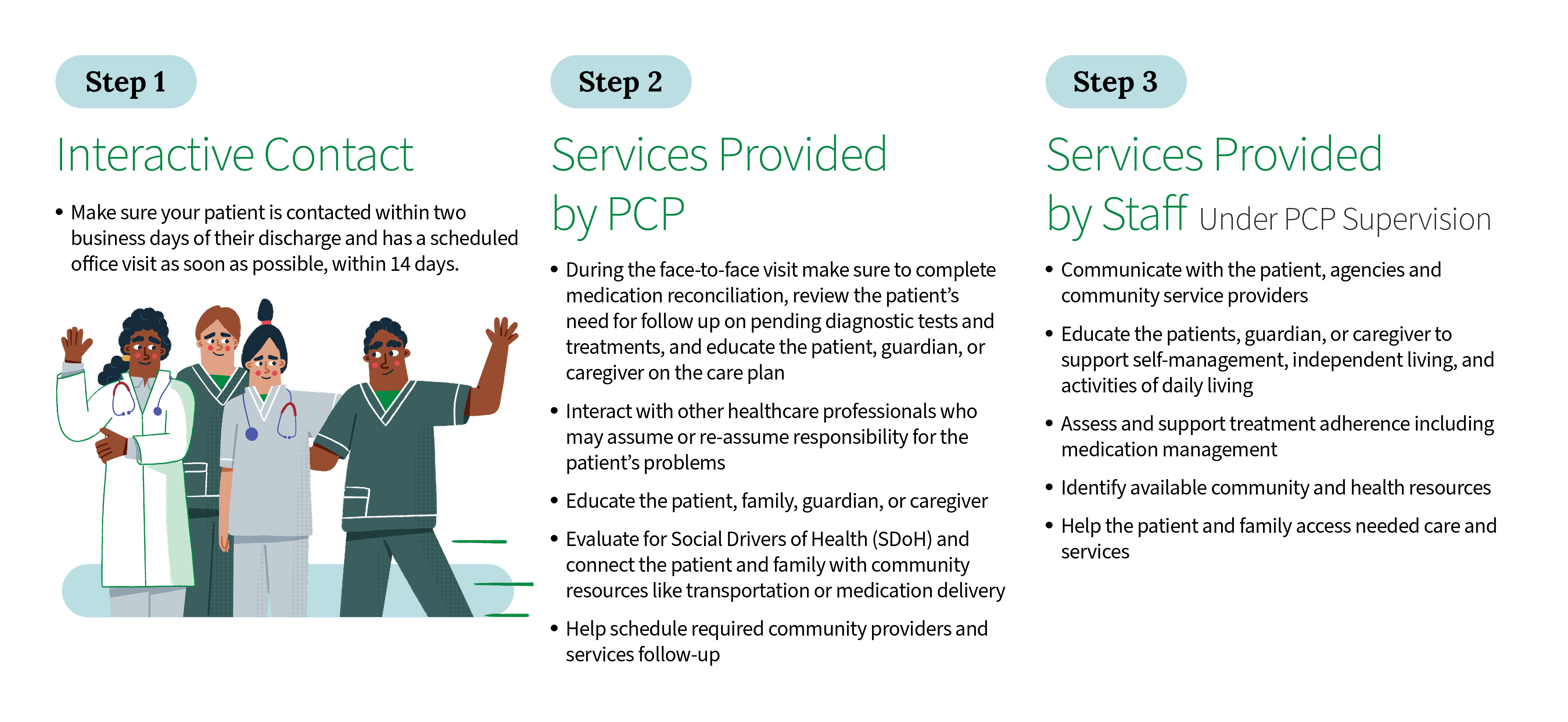
Transitional Care Management (TCM) services are offered during the 30-day post-discharge period to help combat these care gaps. They are covered by Medicare to help patients transition back to the community. TCM visit components include:
What are the benefits of proper ToC
Patients:
- Provide for dedicated time for the PCP to provide education to the patient about his/her medical condition and what brought him/her to the hospital in the first place
- Allow time for medication reconciliation, reviewing medications that were either stopped or started in the hospital, as well as medications that had dosage or frequency changes to ensure that patients are taking medications safely and appropriately
- Coordinate follow up care with specialists as needed for the patient, as well as assist in setting up community resources that are necessary for a full recovery
- Reduce hospital readmissions
Providers:
- Continue to build that relationship and trust that prompts the patient to call the provider when he/she needs medical guidance the most
- Provide PCPs financial support through greater CMS reimbursements
- Post hospital visits drive savings by reducing readmissions
Population:
- Patient is less likely to be readmitted to the hospital.
- This will reduce readmission rates and reduce overall costs for the ACO patient population.
To continue learning about how to drive success in value-based care contact us today!