Why Primary Care Clinicians Should Consider a Population Health Approach to Chronic Kidney Disease
March is National Kidney Month. Currently, there are approximately 37 million American adults affected by chronic kidney disease (CKD) — most of whom are aged 65 years old and older.
 How can providers play a role in early detection and management of CKD?
How can providers play a role in early detection and management of CKD?
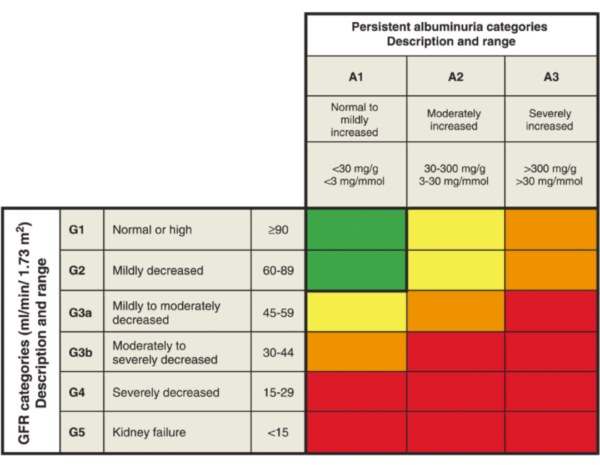
Population-based screening for CKD is not currently recommended, yet it is estimated that 90% of patients with CKD are unaware they have the chronic condition. Screening patients at risk of CKD using eGFR and urine: albumin to creatinine ratio, a key indicator of prognosis, with common risk factors such as hypertension and diabetes will lead to earlier disease detection. The presence of two abnormal lab values across three months distinguishes between acute injury and chronic disease.
The prognosis of CKD by eGFR and albuminuria categories: KDIGO 2012
The four interventions that reduce CKD progression are:
- Blood pressure control <140/90 mm Hg
- Use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers for albuminuria and hypertension
- Diabetes control
- Correction of metabolic acidosis
CKD Risk and Disparities
CKD disproportionately affects minority populations. Among Medicare fee-for-service enrollees in 2020, Black Americans were most heavily affected by CKD (36%), followed by American Indian/Alaska Natives (32%), Hispanic Americans (29%), and Asian Americans/Pacific Islanders (26%).
Racial and ethnic minorities are also more likely to progress from CKD to end-stage renal disease (ESRD) and are less likely to have been under the care of a nephrologist before starting dialysis. These disparities are related to patient, clinician, clinical and system factors.
The Role of Primary Care in CKD Management and Health Equity
Compared to patients whose chronic kidney disease remains unknown, those with chronic kidney disease diagnosed by a primary care clinician are more likely to avoid risky use of non-steroidal anti-inflammatory drugs (NSAIDs); use angiotensin-converting-enzyme inhibitors (ACE-Is) or angiotensin receptor blockers (ARBs) when indicated; and receive appropriate nephrology referrals.
Primary care practice teams can help reduce disparities in care for CKD through early identification, treatment, monitoring progression, collaborating with nephrologists and other specialists, building care teams and engaging patients.
If you are interested in creating a population health-based CKD program, you will see some of the steps outlined below:
 Visit CMS.gov to learn more.
Visit CMS.gov to learn more.
We salute all Vytalize primary care partner practices who screen high-risk groups for CKD and follow evidence-based guidelines in their management. If you are interested in working with a value-based partner to improve clinical outcomes and health equity for your patients with CKD or any other chronic disease, contact us here.